How the overtreatment of diabetics may have cost lives
A brief period in which British family doctors were offered a financial inducement to treat diabetic patients more intensively could be coming to an end.
Not a moment too soon, according to critics who warned that the tougher targets introduced in 2009 would do more harm than good.
The advisory committee that sets the targets doctors must hit in order to maximise their earnings has decided to relax this one for fear of “unintended consequences” (read: damage to patients’ health, or even death).
In 2009, the Quality and Outcomes Framework (QOF) governing financial incentives for GPs was altered. Doctors were told that they should treat patients intensively enough to reduce their blood glucose level, measured by an index called HbA1c, to 7.0 per cent, rather than the previous target of 7.5 per cent. (see footnote for a definition of HbA1c.)
This guidance came in the face of well-informed criticism, and published evidence from trials, that showed no benefit and some risk of harm in what was proposed.
The committee has now done a U-turn, recommending the target be restored to 7.5 per cent, and conceding there is sufficient “uncertainty” about patient safety to justify the move. The 7.0 per cent target “has almost certainly caused harm to patients” says Dr Richard Lehman, a Banbury GP who was among those who cautioned against its adoption.
If a new drug had been licensed, given to hundreds of thousands of patients in spite of evidence of potential harm, then withdrawn after a year, the press would be howling for the blood of those responsible. But when the damage is done by a mistaken guideline, and backed by the Government’s own financial incentives to GPs, the silence is deafening.
Diabetes is a huge and growing problem, with 2.6 million people in the UK diagnosed with the condition, and another half million undiagnosed (according to Diabetes UK figures). The great majority are type 2 (or “adult onset”) diabetics, to whom this guidance referred. Overall prevalence is around 4.5 per cent, which means that an average GP practice with a list of 6,000 would be treating 250-300 such patients. The potential impact of a guideline, if dutifully followed by GPs, is huge.
A non-diabetic has an HbA1c value of around 4.0 to 6.0. Anything over 6.5 is generally taken to be diagnostic of diabetes, and those who fall just below this are sometimes described as having “prediabetes”, with strong pressure from drug companies that they, too, should be treated with drugs to bring down the glucose levels in their blood.
At issue is how low the target should be set. Enthusiasts for treatment say the lower the better. Two members of the group that proposed the reduction to 7.0 per cent, Simon Griffin and Jonathan Graffy from Cambridge, said doctors “can have confidence that the modest changes encouraged by the revised QOF targets are safe and will lead to further reductions in risk and health service costs over time”. (Dr Griffin is assistant director of the MRC Epidemiology Unit and Dr Graffy is a researcher from the General Practice and Primary Care Research Unit.)
To earn the average practice £3,000 a year, half its patients with type 2 diabetes would have to have their HbA1c reduced to less than 7.0 per cent. That meant that many thousands of patients would need more powerful prescriptions, or to switch to insulin therapy if drugs proved unable to get them below the target.
Yet when this new target was being agreed in October 2008, two large studies had just been published showing that intensive HbA1c reduction in established type 2 diabetes had little benefit and could be harmful. The ACCORD trial was terminated early because of higher mortality in the intensively-treated group, while the ADVANCE trial showed no significant difference in all-cause mortality between those treated to an HbA1c of 6.5 per cent and those treated to 7.5 per cent.
These trials were no secret. In September 2008, the month before the 7.0 per cent target was agreed, the National Prescribing Centre (an NHS body) reported on the two studies, saying that they had been “unable to identify a significant improvement in important patient-related outcomes with intensive therapy”.
An editorial in BMJ, published in March 2009 by Dr Lehman and Professor Harlan Krumholz of Yale University, had made the same point (1). “The new QOF target encourages an outdated strategy and one that may not provide a net benefit to patients” it concluded. “The change of target from 7.5 per cent to 7.0 per cent should be withdrawn before it wastes resources and possibly harms patients.”
There have since been further studies confirming the point. In April, The Lancet published a study (2) of nearly 48,000 patients from the UK General Practice Research Database whose intensity of treatment had been increased. Of these, 27,965 were given more powerful drugs and 20,005 had been switched to insulin therapy. The outcome measure was death from all causes.
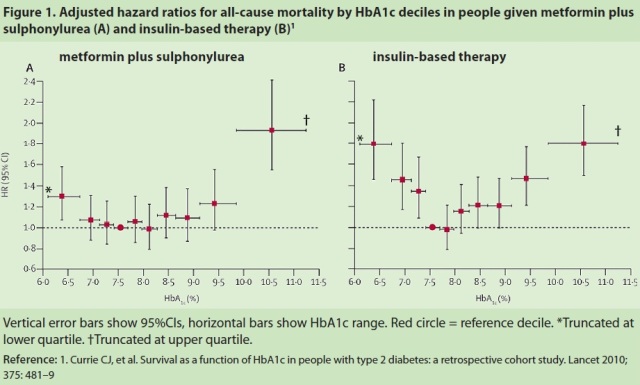
This study, by Dr Craig Currie of Cardiff University School of Medicine and colleagues, showed that deaths followed a U-shaped curve, with minimum mortality in patients at an HbA1c score of 7.5 per cent. Scores higher or lower than that led to increased deaths, especially among patients on insulin therapy.
The difference in deaths between 7.5 per cent and 7.0 per cent was 9 per thousand in the drug-treated group and 70 per thousand in the insulin-treated group. (The groups chosen in the study do not conform precisely to the 7.5 or 7.0 scores, but these are the closest.) The figure below is taken from the study.
The cause of the additional deaths remains unclear, but intensive glucose control can lead to hypoglycaemia (very low glucose levels) which in turn is linked to heart rhythm disturbances. Heart attacks are another possible cause of death, as is kidney failure and possibly cancer in the insulin-treated patients. But the study, funded by the drug company Eli Lilley, did not set out to determine what caused the additional deaths.
Nor can it tell us how many may have died as a result of the QOF guideline, because that would depend on how many patients were switched to insulin therapy to achieve it. However, spending on prescriptions for diabetes surged in 2009-10 by 8.3 per cent. Overall, diabetic drugs accounted for 7.7 per cent of GP prescribing in 2009-10, compared to 5.8 per cent in 2004/5.
In fact, the existing NICE guideline calls for 6.5 per cent HbA1c, even further away from the level the evidence suggests is ideal. (NICE guidelines and the guidelines NICE helps produce for QOF are not identical. Why? Don’t ask.)
And evidence cited by Drs Griffin and Graffy suggests that many diabetics have been intensively treated. In the 2005-06 national diabetes audit, they say, 45 per cent had values of 7.0 per cent or less.
All this suggests that, driven by NICE and QOF guidelines, hundreds of thousands of patients have been treated in a way that was not in their best interests. Many may have died as a result.
Mistakes over guidelines are understandable, even if they are supposed to be evidence-based. GPs fortunately use their discretion in interpreting them. But it is hard to stomach GPs being paid extra to meet a guideline that risked damaging their patients’ health, when experts had pointed out the risks in advance.
In fact, it’s unconscionable. When will somebody point this out in the mainstream media?
References
1.Tight Control of blood glucose in long standing type 2 diabetes, by Richard Lehman and Harlan M Krumholz, BMJ 2009;338:b800
2. Survival as a function of HbA1c in people with type 2 diabetes: a retrospective cohort study, by Graig J Currie, John R Peters, Aodan Tynan, Marc Evans, Robert J Heine, Oswaldo L Bracco, Tony Zagar and Chris D Poole, Lancet 2010; 375; 481-89
Footnote: In the bloodstream glucose is bound to the haemoglobin to make a glycosylated haemoglobin molecule, called haemoglobin A1c or HbA1c. The more glucose in the blood, the greater the quantity of HbA1C measured as a percentage of total haemoglobin. But don’t bother to memorise this: from 1 June a different scale has been in use in the UK, as mmol per mol of free haemoglobin. The old 7.0 per cent measure equals 53 mmol/mol, while 7.5 equals 59. An explanation is available here.




Anonymous (not verified) wrote,
Wed, 11/08/2010 - 10:26
would the reduction [and financial incentive] have been introduced to give benefits to some patients? by focussing on possible adverse effects for some others and suggesting the impact may have been to cause actual deaths, without any evidence at all to support that (for example from coroners), you are scare-mongering in a much worse way than the tabloids - by presenting a pseudo scientific argument, it appears more persuasive. The arguments over whether the guidance is right or wrong are nothing to do with whether gps are being paid to follow them, if death had been caused by gps following them and not paid it would have been no less serious would it? So again you are being sensationalist
the fact is that all treatments and all guidance carries risks which are not always known or well quantified in advance - and to suggest otherwise is just bad science. if regulators always avoid every risk in developing new guidelines they will also avoid lots of benefits.
please try to be more measured and balanced, using evidence to support your arguments, not speculation and sensationalism, in future.
GF (not verified) wrote,
Wed, 11/08/2010 - 13:30
Anonymous: Did you read the same article as me? The guidance is wrong (and was demonstrably wrong) AND GPs were paid to follow it. This is a double scandal.
Why on earth are coroners' reports needed to prove deaths were caused? In the trials deaths were higher; why are normal non-trial patients different?